
Opioids are a class of drugs that interact with receptors on nerve cells in the body and brain. Opioids include pain relievers as well as illicit street drugs.

When taken, it can make the user feel euphoric and pain-free. Therefore, opioids can become highly addictive drugs. Some opioids, such as heroin, are illegal. However, many opioids are legal and are prescribed by health care providers to treat pain; these include oxycodone (OxyContin®), hydrocodone (Vicodin®), hydrocodone-acetaminophen (Norco®), oxycodone-acetaminophen (Percocet®). codeine, and morphine, among others. Use of these prescription drugs for short durations, as prescribed by a doctor, is generally safe. However, misuse of prescription opioids can lead to addiction and even overdose or death. Misuse can include taking a drug that has been prescribed for someone else, taking a prescribed medicine differently than prescribed (for example, at a higher dose or for a longer period of time), or taking it to get high. SOURCE: https://www.hhs.gov/ash/oah/adolescent-development/substanceuse/drugs/opioids/index.html
Many people are prescribed medication when they have injured themselves or after a surgery. Frequently, these medications are prescription opioids. Prescription opioids can be very effective at reducing pain, and, for some people, improve their quality of life and ability to function.


Opioids are a class of drugs that include powerful pain relievers that are available by prescription, such as oxycodone (OxyContin®), hydrocodone (Vicodin®), as well as illegal drugs such as heroin. These drugs are chemically related and have similar effects on the brain and body.
Heroin is an illegal opioid drug made from morphine, a natural substance taken from the seed pod of the various opium poppy plants. Heroin can be a white or brown powder, or a black sticky substance known as black tar heroin.

People inject, sniff, snort, or smoke heroin. Some people mix heroin with other drugs. It is highly addictive. People who regularly use heroin often develop tolerance, which means that they need higher and/or more frequent doses of the drug to get the desired effects.
A person can overdose on heroin. A heroin overdose occurs when a person uses enough of the drug to produce a life-threatening reaction or death.
Opioid pain relievers are generally safe when taken for a short time and as prescribed by a doctor. However, because they produce euphoria in addition to pain relief, they can be misused (taken in a different way or in a larger quantity than prescribed, or taken without a doctor's prescription). Regular use - even as prescribed by a doctor - can lead to dependence and, when misused or overused, opioid pain relievers can lead to addiction, overdose, and death.

Prescription opioid pain medicines such as oxycodone and hydrocodone have effects similar to heroin. Research suggests that misuse of these drugs may open the door to heroin use. Nearly 80 percent of Americans using heroin (including those in treatment) reported misusing prescription opioids first. Talk to your doctor if you currently have a prescription for opioids.
Fentanyl is a powerful synthetic opioid that is up to 100 times more potent than morphine and 50 times more potent than heroin. It is both a prescribed drug, as well as a drug that is at times made and used illegally.
Prescription fentanyl is typically used to treat patients with severe pain, especially after surgery. It is also sometimes used to treat patients with chronic pain who are physically tolerant to other opioids.
Fentanyl that is illegally manufactured is dangerous. It is made without the quality controls of pharmaceutical grade fentanyl and is a major contributor to recent increases in synthetic opioid overdose deaths. This illegally manufactured fentanyl is sold illegally as a powder, dropped onto blotter paper, put in eye droppers and nasal sprays, or made into counterfeit pills that look like other prescription opioids.
Importantly, some drug dealers are mixing fentanyl with other drugs, such as heroin, cocaine, methamphetamine and MDMA. This is especially risky when people taking drugs don't realize that the drugs they are using might contain fentanyl and significantly increase their risk for overdose death.


If you're one of millions of Americans with long-term pain, also called chronic pain, you know how debilitating and frustrating it can be. It can be harmful to your health and well-being. It can keep you from getting a good night's sleep, eating right, and exercising. It can affect your mood and work, and can keep you from spending time with your friends and family.
Every year, millions of prescriptions are written for pain medications - many of them are opioids that can lead to addiction. But there are many other treatments available for pain instead of opioids that may work better and have fewer associated risks.
The Dangers of Taking Prescription Opioids Recreationally
It's dangerous to take prescription pain medications recreationally or for reasons other than managing pain as directed.
It can lead to addiction and unintentional overdose. Taking opioids with alcohol or sedatives increases the risk of overdose. Misuse of prescription opioids is also a risk factor for transitioning to heroin use.
Talk to your doctor about trying these non-opioid alternatives for pain relief.
Non-Opioid Medication Options
| Medication | Examples | Indications | |
|---|---|---|---|
| Over-the-Counter (OTC) |
Acetaminophen | Acetaminophen (Tylenol®) | Osteoarthritis, chronic lower back pain, migraine |
| Non-Steroidal AntiInflammatory Drugs |
Ibuprofen (Motrin®, Advil®, Aleve®), Celecoxib (Celebrex®) |
Acute and chronic low back pain, osteoarthritis |
|
| Topical Agents | Capsaicin | Neuropathic pain, osteoarthritis, musculoskeletal pain |
|
| Requires a Prescription |
Tricyclic Anti-Depressants | Amitryptyline (Elavil®, Endep®), Nortriptyline (Pamelor®) |
Diabetic neuropathy, post-herpetic neuralgia, fibromyalgia, migraine |
| Anticonvulsants | Pregabilin, Gabapentin, Carbamazepine | Diabetic neuropathy, postherpetic neuralgia, fibromyalgia | |
| Topical Agents | Lidocaine, Topical Non-Steroidal Anti-Inflammatory Drugs | Neuropathic pain, osteoarthritis, musculoskeletal pain | |
| Interventional Approaches | Epidural or Joint Injections | Glucocorticoid injections | Osteoarthritis, Rheumatoid arthritis, rotator cuff disease |
Non-Pharmacological Treatment Options
| Treatment | Indications |
|---|---|
| Physical/Exercise Therapy | Lower back pain, fibromyalgia, osteoarthritis |
| Cognitive Behavioral Therapy (CBT) | Chronic pain, disability, mood |
| Acupuncture | Chronic pain, fibromyalgia |
| Therapeutic massage | Chronic pain, fibromyalgia |
Each of these treatment options may have risks. Talk to your doctor about what the potential risks could be.
For more information on safe opioid prescribing, review Safe Med LA's Safe Opioid Prescribing Recommendations (endorsed by the California Society of Addiction Medicine).
Making decisions about treating pain is difficult. If you are considering starting or questioning whether to continue taking prescription opioids, talk to your doctor about side effects, risks, and addiction - and make sure that you watch for them too.
Here are a few questions that can help you and your doctor make the best choice for you:


Naloxone
Ask your doctor about naloxone - a safe medication that can quickly stop an opioid overdose. It can be injected into the muscle or sprayed into the nose to rapidly block the effects of the opioid on the body.
Naloxone is a medicine that can treat an opioid overdose when given right away. It works by rapidly binding to opioid receptors and blocking the effects of heroin and other opioid drugs. Sometimes more than one dose may be needed to help a person start breathing again, which is why it's important to get the person to an emergency department or a doctor to receive additional support if needed.
Naloxone is available as an injectable (needle) solution, a handheld auto-injector (EVZIO®), and a nasal spray (NARCAN® Nasal Spray). You don't have to be a health care professional to give naloxone. Friends, family, and others in the community who receive the right training can use it to save someone who is overdosing.
The rising number of opioid overdose deaths has led to an increase in public health efforts to make naloxone available to at-risk persons and their families, as well as first responders and others in the community. California allows pharmacists to dispense naloxone without a prescription from a person's personal doctor.
For additional information and training on how to use naloxone in response to an opioid overdose, click here.

All adolescents are at risk for misusing opioids. There are a number of concrete ways that parents, family members, and other concerned adults can help prevent opioid misuse among adolescents. The fact that the adolescent brain is still growing means that teens are vulnerable to addiction, but the adolescent brain also is ripe for learning healthy habits and behavior.
To help prevent opioid misuse, those who care about and for adolescents should:

Key Los Angeles County Statistics
 Source: CDC Wonder
Source: CDC Wonder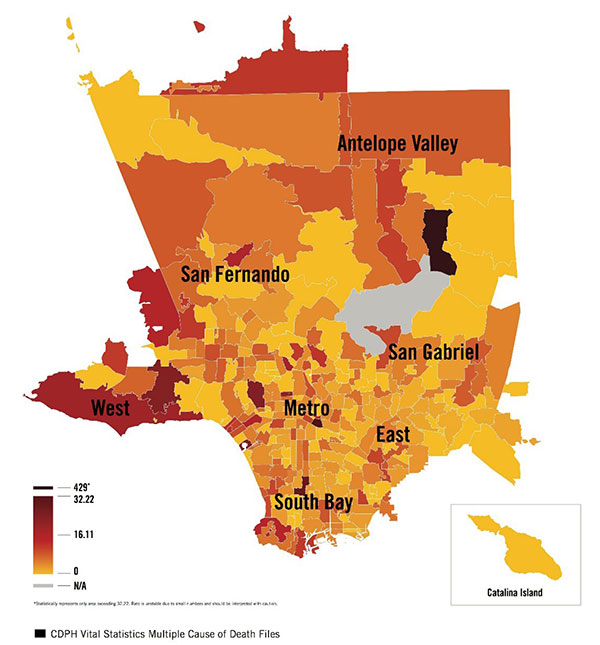 Source: CDPH Vital Statistics
Source: CDPH Vital Statistics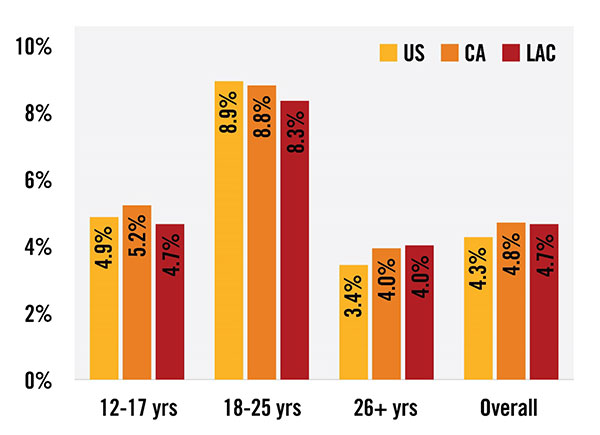 Source: SAMHSA
Source: SAMHSA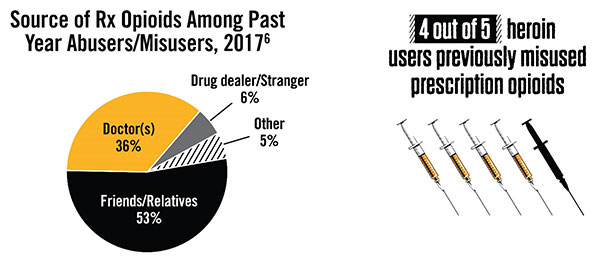 Source: SAMHSA
Source: SAMHSA Source: SAMHSA
Source: SAMHSA
There is more than one path to recovery. MAT is a proven treatment for opioid use disorders that uses medications such as methadone or buprenorphine to treat addiction to both illegal opioids and prescription opioids. MAT works by both relieving cravings for opioids and staving off withdrawal symptoms so that people can focus on their recovery.
Talk to your doctor about whether MAT is right for you.
For more information on MAT, click here.

Heroin is an opioid drug made from morphine, a natural substance taken from the seed pod of the various opium poppy plants grown in Southeast and Southwest Asia, Mexico, and Colombia. Heroin can be a white or brown powder, or a black sticky substance known as black tar heroin. People inject, sniff, snort, or smoke heroin. Some people mix heroin with crack cocaine, a practice called speedballing.
Heroin enters the brain rapidly and binds to opioid receptors on cells located in many areas, especially those involved in feelings of pain and pleasure and in controlling heart rate, sleeping, and breathing.

The Dangers of Heroin
Heroin is addictive and there is a high risk of overdose and death from using it.
Heroin also often contains additives, such as sugar, starch, or powdered milk, that can clog blood vessels leading to the lungs, liver, kidneys, or brain and cause permanent damage.
In addition, sharing drug injection equipment and having impaired judgment from drug use can increase the risk of contracting infectious diseases such as HIV and hepatitis (see "Injection Drug Use, HIV, and Hepatitis").
Risk of Overdose
A person can easily overdose on fentanyl. An overdose occurs when a drug produces serious adverse effects and life-threatening symptoms. Death from an opioid overdose happens when the drug depresses the parts of the brain that control breathing. Signs and symptoms when people overdose on opioids include
Risk of Addiction
Heroin is highly addictive. People who regularly use heroin often develop tolerance, which means that they need higher and/or more frequent doses of the drug to get the desired effects.
Those who are addicted to heroin and stop using the drug abruptly may have severe withdrawal. Withdrawal symptoms - which can begin as early as a few hours after the drug was last taken - include:
Researchers are studying the long-term effects of opioid addiction on the brain. Studies have shown some loss of the brain's white matter associated with heroin use, which may affect decision-making, behavior control, and responses to stressful situations.

For more information, see our brochure (PDF): English | Spanish
No Cost, No Fee Treatment for Substance Use Disorders
People who have a Substance Use Disorders (also known as addiction) may be eligible to receive no cost treatment for opioid or other drug addiction. For more information or to see if you are eligible, call the number above or click here.

Addiction is a complex condition, a brain disease that is manifested by compulsive substance use despite harmful consequences. People with addiction have an intense focus on using a certain substance(s), such as alcohol or drugs, to the point that it takes over their life. They keep using alcohol or a drug even when they know it will cause problems.
Dependence develops when the neurons in the body adapt to the repeated exposure of the substance and only function normally in the presence of the substance. When the substance is withdrawn, several physiologic reactions occur. These can be mild (e.g., for caffeine) or even life threatening (e.g., for alcohol). This is known as the withdrawal syndrome.
Drug misuse is improper or unhealthy use of a drug. These include the repeated use of drugs to produce pleasure, alleviate stress, and/or alter or avoid reality. It also includes using prescription drugs in ways other than prescribed or using someone else's prescription.
Opioid Use Disorder, sometimes referred to as "opioid abuse or dependence" or "opioid addiction," is a problematic pattern of opioid use that causes significant impairment or distress.
Opioids are a class of drugs that include the illegal drug heroin, synthetic opioids such as fentanyl, and pain relievers available legally by prescription, such as oxycodone (OxyContin®), hydrocodone (Vicodin®), codeine, morphine, and many others.
Fentanyl is a powerful synthetic opioid analgesic that is similar to morphine but is 50 to 100 times more potent.
Heroin is an opioid drug made from morphine, a natural substance taken from the seed pod of the various opium poppy plants grown in Southeast and Southwest Asia, Mexico, and Colombia. Heroin can be a white or brown powder, or a black sticky substance known as black tar heroin.
Naloxone is a short-acting medication that reverses the life-threatening effects of an opioid overdose.
Medication-assisted treatment (MAT) is the use of medications with counseling and behavioral therapies to treat substance use disorders and prevent opioid overdose.
Recovery is a process of change through which people improve their health and wellness, live self-directed lives, and strive to reach their full potential. There are four major dimensions that support recovery:

If you are providing care for a patient or a family member who is taking a prescription opioids for pain, it is important that you are aware of the potential risks associated with their medication. These include the potential risk of dependency, addiction, overdose, and death, as well as how to prevent overdose.
When talking to your patient or family member's doctor about prescription pain medications, ask the following questions:

What do I need to know about dependency and addiction?
It may not be easy to tell if someone is becoming addicted to prescription opioids. Perhaps you've noticed changes in your patient's or loved one's moods or behavior that don't add up.
Even if you can't point to anything specific, addressing your concerns could save their life
Taking opioids as prescribed reduces the likelihood someone will become addicted. However, not taking prescription opioids as prescribed or for an extended period of time increases the risk of misuse, addiction, overdose, and death. Studies suggest that up to one-third of people who take opioids for chronic pain misuse them, and more than 10 percent become addicted over time.
Your patient or loved one is also at increased risk of addiction if he or she obtains opioids without a prescription, and using opioids illegally increases the risk of drug-related death. Drugs that pass hands illegally, such as fentanyl may be laced with life-threatening contaminants or much more powerful opioids. And people who use opioids illegally often turn to heroin, which is a cheaper alternative to prescription opioids that has similar effects.
Signs of misuse, dependency and addiction
People who are addicted to opioids may still hold down jobs and other responsibilities, maintaining the appearance of stability at work and home.
Over time, however, the addiction is likely to lead to serious problems. When a person is addicted to a drug, he or she will continue to use the drug even when it makes his or her life worse.
Common signs of opioid addiction include:
If someone you love is addicted to opioids, you're also likely to experience changes in your thoughts and behaviors. You may find yourself:
It's common - and entirely human - to avoid addressing your concerns for fear your relationship or family will fall apart. Some addiction experts now recommend that doctors interview family members and caregivers as part of routine follow-up care for a person taking opioid medications. But don't wait to be asked before you voice your concerns. If you think your loved one may be addicted to opioids, talk with his or her doctor right away.
Preventing Overdose
Death from an opioid overdose happens when too much of the drug overwhelms the brain and interrupts the body's natural drive to breathe. Signs and symptoms when people overdose on opioids includes:
It may be hard to tell if a person is high or experiencing an overdose. If you aren't sure, it's best to treat it like an overdose - you could save a life.

Fentanyl is a powerful synthetic opioid that is up to 100 times more potent than morphine and 50 times more potent than heroin. It is both a prescribed drug, as well as a drug that is at times made and used illegally.
 Like morphine, prescription fentanyl is typically used to treat patients with severe pain, especially after surgery. It is also sometimes used to treat patients with chronic pain who are physically tolerant to other opioids. When prescribed by a doctor, fentanyl can be given as a shot, a patch that is put on a person's skin, or as lozenges that are sucked like cough drops.
Like morphine, prescription fentanyl is typically used to treat patients with severe pain, especially after surgery. It is also sometimes used to treat patients with chronic pain who are physically tolerant to other opioids. When prescribed by a doctor, fentanyl can be given as a shot, a patch that is put on a person's skin, or as lozenges that are sucked like cough drops.
Fentanyl that is illegally manufactured is dangerous. It is made without the quality controls of pharmaceutical grade fentanyl and is a major contributor to recent increases in synthetic opioid overdose deaths. This illegally manufactured fentanyl is sold illegally as a powder, dropped onto blotter paper, put in eye droppers and nasal sprays, or made into counterfeit pills that look like other prescription opioids.
Importantly, fentanyl is also being mixed with other drugs, such as heroin, cocaine, methamphetamine, and MDMA. This is especially risky when people taking drugs don't realize that the drugs they are using might contain fentanyl and significantly increase their risk for overdose death.
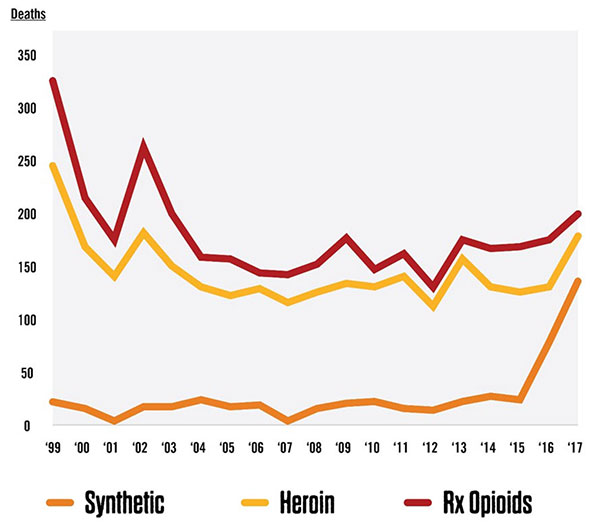
Synthetic opioids, including fentanyl, are now the most common drugs involved in drug overdose deaths in the United States. In 2017, 59 percent of opioid-related deaths involved fentanyl, compared to 14.3 percent in 2010.
Risk of Addiction
Fentanyl is addictive because of its potency. A person taking prescription fentanyl as instructed by a doctor can still experience dependence, which is characterized by withdrawal symptoms when the drug is stopped. A person can be dependent on a substance without being addicted, but dependence can sometimes lead to addiction.
People addicted to fentanyl who stop using it can have severe withdrawal symptoms that begin as early as a few hours after the drug was last taken. These symptoms can be extremely uncomfortable and are the reason many people find it so difficult to stop taking fentanyl.
These symptoms include:
